RENUKA RAI
Thimphu
Bhutan is intensifying its efforts to combat tuberculosis (TB) with a combination of advanced diagnostic tools, artificial intelligence-assisted screenings, and shorter treatment regimens.
As part of its commitment to the global End TB Strategy, the government aims to reduce TB incidence by 80% and TB-related deaths by 90% by 2030.
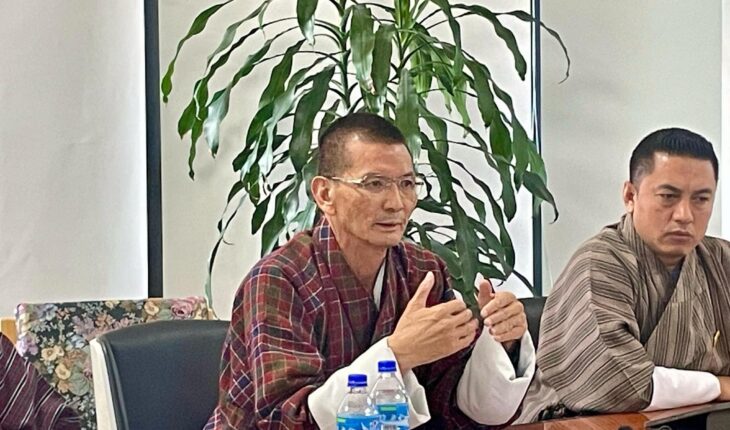
During the meet the press session on 1 April, Secretary of Health, Pemba Wangchuk, emphasized the urgency of tackling the disease. “TB remains a major public health challenge, but with the latest advancements in diagnostics and treatment, we have an opportunity to significantly reduce its burden. Our goal is not just to treat TB but to eliminate it as a threat to our communities,” he said.
A crucial part of the strategy is improving early and accurate TB detection. The Ministry of Health has expanded the use of GeneXpert machines, which can rapidly diagnose TB and detect drug-resistant strains such as Multi-Drug Resistant TB (MDR-TB) and Extensively Drug Resistant TB (XDR-TB) in just a few hours.
These machines, now available at 17 sites across the country, are expected to reduce diagnostic delays and ensure that patients receive timely treatment.
In addition, the country is set to introduce the Cy-TB test in 2025, a next-generation skin test designed to detect latent TB infections—cases where individuals carry the bacteria but do not yet show symptoms. The health ministry believes that diagnosing and treating latent TB before it becomes active will be key to reducing transmission in the long run.
Artificial intelligence is also being integrated into Bhutan’s TB detection strategy. The country is leveraging Qure AI technology, an AI-powered screening tool that enhances the accuracy and efficiency of TB detection, particularly in remote areas where access to medical facilities is limited.
“With AI-assisted diagnostics, we can identify cases faster and more accurately, even in the most remote regions of Bhutan. This is a game-changer in our fight against TB,” Secretary Pemba Wangchuk added.
To ensure that no TB cases go undetected, MoH has strengthened its contact tracing efforts, focusing on individuals who have been in close contact with TB patients. Mobile TB screening and testing units are also being deployed to reach high-risk and vulnerable populations, including people living with HIV, migrant workers, prisoners, and young children.
Furthermore, health officials are particularly targeting overcrowded settings, such as dormitories and shared kitchens, where TB transmission is more likely.
MoH is also improving treatment options by adopting shorter, all-oral TB treatment regimens, following recommendations from the World Health Organization (WHO). Under the new guidelines, patients with drug-susceptible TB will receive treatment for four to six months, compared to the conventional six to nine months.
For those diagnosed with MDR-TB, the treatment period has been reduced to six months, down from the previous nine to eleven months
The shorter regimens are expected to improve patient adherence, reduce side effects, and increase treatment success rates. The Ministry of Health has also introduced a comprehensive follow-up system, in which healthcare workers conduct home visits, make phone calls, and send SMS reminders to ensure patients complete their treatment.
The health secretary stressed the importance of these changes. “One of the biggest challenges in TB treatment is ensuring that patients complete their full course of medication. These new regimens will make it easier for patients to adhere to treatment, ultimately saving lives and preventing the spread of drug-resistant TB strains.”
Alongside medical advancements, the government is reinforcing its Directly Observed Treatment (DOT) program, where healthcare workers or trained community volunteers supervise patients taking their medication. This initiative has been instrumental in preventing drug resistance and ensuring that patients complete their treatment successfully.
Nationwide public awareness campaigns are also being launched to educate citizens about TB symptoms, the importance of early detection, and the availability of free treatment. By addressing misconceptions and reducing the stigma surrounding TB, Bhutan hopes to encourage more people to seek medical help at the earliest signs of infection.
Health Secretary Pemba Wangchuk expressed confidence in Bhutan’s ability to make significant progress. “We have the technology, the expertise, and the commitment of our healthcare workers. But we also need the support of our communities. If we work together, we can achieve a future where TB is no longer a threat to our people.”
Despite medical advancements, TB remains one of the top 10 infectious causes of death worldwide. The disease is caused by the bacterium Mycobacterium tuberculosis and spreads through the air when an infected person coughs or sneezes. While TB primarily affects the lungs (Pulmonary TB), it can also infect other parts of the body (Extra-Pulmonary TB).
Many individuals carry the infection in a latent state, meaning they show no symptoms but may develop the disease later. People with weakened immune systems, such as those who are malnourished or living with HIV, face a much higher risk of developing active TB.
The other strategy is to strengthening community-based healthcare initiatives, such as Directly Observed Treatment(DOT), to improve treatment adherence through ambulatory care models and aggressive awareness campaigns are being conducted to reduce stigma and educate the public about TB symptoms and the importance of timely treatment.
Bhutan’s commitment to fighting TB through advanced diagnostics, AI-powered screenings, improved treatment, and strong community engagement marks a significant step toward eliminating the disease. With continued investment and public cooperation, the country is well on its way to achieving its 2030 End TB targets and securing a TB-free future.